The Transplant Process (Autologous)
New Patient Consult/Insurance Verification
↓
Pre-Transplant Evaluation
↓
Insurance Authorization / Approval
↓
Informed Consent Conference
↓
Start of Zarxio / Mobilization
↓
Have a Central Venous Line Placed
↓
Collect Stem Cells through Apheresis
↓
Receive Transplant Preparative Regimen (Chemotherapy)
↓
Receive Your Stem Cell Transplant
↓
Wait for Engraftment
The Transplant Process
Our BMT nurse coordinators and care team will help you through the transplant process. We understand each patient’s situation is different. This information will give a basic summary of the transplant process.
New patient consult and insurance verification
The first step is an initial visit with one of our transplant physicians. They will make an individualized plan for your disease. You will also meet your pre-transplant coordinator to start the process of finding the best donor for you.
A transplant financial coordinator will meet with you at your first clinic visit. Your transplant financial coordinator will take your insurance information. They will then determine if you can have a transplant at our cancer center. They will check your insurance policy and make sure that transplant is covered. They will give yo their contact information for questions.
Pre-transplant evaluation
When a donor has been found and you are ready to start the transplant process, you will have a series of tests done. This initial evaluation is done at the outpatient clinic. The pre-transplant evaluation is tests that assess your specific disease, staging, and general health. This is done to make sure your body is able to tolerate high doses of chemotherapy. Some of these tests may be required by your insurance for transplant approval. They may need to be repeated again prior to transplantation. This is to make sure there is no new disease and to provide a baseline for comparison after the transplant.
The schedule for the days of testing can be busy and full. We do this to make the most of your time so you do not have to drive back and forth to get all testing completed.
Tests typically done during the pre-transplant evaluation:
- Bone marrow biopsy and aspirate:
- A needle is inserted into the bone to remove marrow to look at flaws in blood cells.
- Laboratory blood work:
- Multiple labs, which includes HIV (Human immunodeficiency virus) and hepatitis screening
- Electrocardiogram (ECG):
- Measures the electrical activity of the heart
- Pulmonary function test (PFT):
- Measures lung function by breathing into a tube connected to a measuring device
- ECHO:
- Looks at heart and heart valve function by using sound waves
- RVG (Radionuclide Ventriculogram or MUGA):
- Measures the strength of the heart muscle
- CT scan (or CAT scan):
- A type of x-ray study that uses computers to obtain a clear picture of the body taken different angles. Sometimes a dye is used to obtain better pictures
- PET scan (Positron Emission Tomography):
- An imaging test that uses short-lived radioactive tracers injected into a vein. The test shows 3D colored images and assesses cell activity and organ function.
- Skeletal survey:
- A skeletal survey is an X-ray to look for bone lesions in selected parts of the skeleton. This is mostly done for patients with multiple myeloma.
- Dental evaluation with X-rays:
- These are done to look for any mouth or dental infections.
- Mammogram:
- You should have a mammogram if you are over 40 or have a family history of breast cancer. You do not need to repeat if you have had one in the last 12 months.
Other appointments will be meeting with the social worker, the dietitian, a psychologist, the palliative care team, and radiation oncology if appropriate. You may be referred to other specialists such as a cardiologist or pulmonologist.
Social Work/Case Management
Social workers are a part of your BMT team. You will be assigned to a BMT social worker in the clinic. Your social worker will be your clinic contact person for concerns and problems related to adjustments to living with a transplant. Some common ways the social worker can help you are:
- Providing a list of lodging options in Kansas City and submitting referrals
- Helping you apply for Social Security disability
- Assisting with private short-term and long-term disability plan forms
- Assisting with Family Medical Leave Act (FMLA) forms
- Coordinating home health services for therapists, medical equipment, and IV medication administration
- Assisting with Advanced Directives
- Providing information on transportation options
- Providing information on how to apply for financial grants, based upon your diagnosis and treatment plan.
You will be assigned a social worker and a nurse case manager in the hospital. They will help you with planning your discharge from the hospital. They always try to meet with you on your day of admission, and then throughout your hospitalization. The hospital social worker helps with many of the same things as the BMT clinic social workers. The nurse case manager will also help coordinate your home health services when you are discharged.
You may have never worked with a social worker or nurse case manager, and are not sure how they can help you. A good rule of thumb is to discuss any problems you are having with your team. If your problem needs the help of a social worker or nurse case manager, the team will contact them to talk with you.
Insurance authorization/approval
We will send the results of your pre-transplant tests to your insurance company for final approval for transplant. You will be notified by the pre-transplant coordinator if any of your tests are abnormal. You may be sent for additional testing. All results will be reviewed at the informed consent conference. Your financial coordinator is available to help you with any financial arrangements and billing issues.
Many commercial insurance companies have their own case managers that work with patients who are having a transplant.
Final approval for transplant will be obtained before you move forward to transplant and related treatment. Notify the transplant financial coordinator immediately of any change or possible change in your insurance. This could impact your approval process.
Informed consent conference
You will be scheduled to review your test results. Please bring at least one of your caregivers with you. You will receive copies of your consent documents before the consent conference. Read all consent documents before your consent conference. The provider will share information so you can make the decision to go ahead with transplant. You and your family will be able to ask questions. After the conference, you or your legal guardian will be asked to sign consent forms. This gives permission to proceed with treatment. Copies of your consent forms and evaluation studies will be given you.
Bring all of your medications with you at the time of your consent conference. These will be reviewed by the pharmacist.
Start of Zarxio / Mobilization and Stem Cell Collection
Stem cells are collected through a process called apheresis. The bone marrow normally has the largest number of stem cells with a very small number circulating in the blood. By increasing the number of stem cells circulating in the blood we are able to collect larger numbers during apheresis (the removal of cells). To get more stem cells into the circulation we will use growth factors to stimulate the marrow.
The growth factor commonly used is called Zarxio (filgrastim). This medication is given subcutaneously (an injection under the skin). It will increase the white blood cell count in the body. The most common side effects of this medication are bone and joint pains, fevers, and headaches. These side effects can be treated with acetaminophen (Tylenol®).You will receive four days of Zarxio and on the fifth day your cells will be collected. This is an outpatient procedure done in our apheresis department at the hospital. You will have this procedure for one to three days in a row for about five hours each day. During apheresis, you may need to stop taking some of your regular medications. Your transplant physician will review your medications and tell you which medications you may need to stop.
If needed, Mozobil (plerixafor) is used with Zarxio (filgrastim) to increase the number of stem cells in your blood. The most common side effects of Mozobil are diarrhea, nausea/vomiting, tiredness (fatigue), injection site reactions, headache, pain in the joints and dizziness. These symptoms can be treated with acetaminophen (Tylenol) and loperamide (Imodium). Symptoms usually go away within two to three days after stopping Mozobil.
Central Venous Catheter
You will be scheduled have a central venous catheter placed. A central venous catheter allows blood to be drawn without having to stick patients in the arm. Please note: certain blood tests cannot be drawn from a catheter. You may receive chemotherapy, IV fluids, and other medications through this type of catheter. We will keep the central catheter in as long as you need it.
Your nurses will help you and your caregiver with your catheter until you feel comfortable caring for it yourself. You will be taught how to flush your catheter and recognize signs and symptoms of potential problems. Detailed care instructions of your central venous catheter will be provided after it is placed.
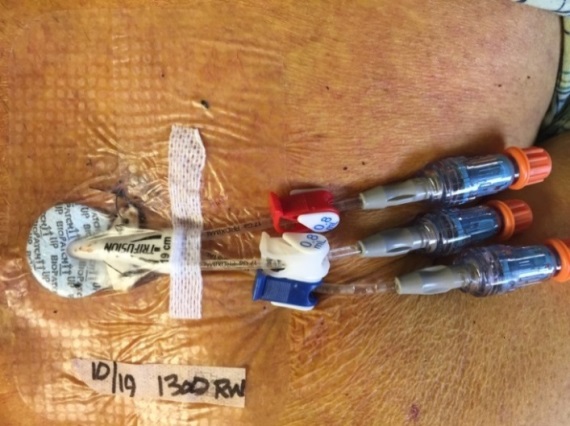
A Trifusion catheter placed in the chest near the neck.
Pre-transplant conditioning
The purpose of chemotherapy before transplant is to kill cancer cells. This makes room in your bone marrow for the transplanted stem cells. The dose of chemotherapy is higher than other chemotherapy treatments you may have had before. There are several pre-transplant conditioning chemotherapy regimens; some also use radiation. Regimens are different depending on the type and stage of cancer. Your physician and pharmacist will discuss medications and doses used to treat your disease.
You will either get your conditioning chemotherapy in the hospital or in the outpatient clinic. However, you will be admitted to the hospital any time you require closer observation.
Potential Side Effects from Pre-Transplant Conditioning
All chemotherapies and radiation have some side effects. Some may be unpleasant. Each drug has different side effects. We will do our best to help manage any side effects that you have.
Some potential side effects from chemotherapy you may have:
- Mouth sores
- Occur because chemotherapy causes cells lining the mouth to die.
- Your nurse may give you ice chips to hold in your mouth while you are getting chemotherapy to prevent mouth sores.
- Nausea and vomiting
- Several medications are available to relieve nausea and keep you comfortable. These medications are called anti-emetics. We will help to find the best possible combination of medications to treat nausea.
- Ask for nutrition assistance if you are having trouble keeping food down.
- Diarrhea
- Stool that is watery and without form.
- Do not take Imodium® (generic: loperamide). unless instructed by the care team
- Hair loss
- Also known as alopecia
- Your hair will typically grow back within 3 to 6 months after stopping chemotherapy.
- Sterility:
- Can be a long-term side effect of high-dose chemotherapy and total body irradiation (TBI)
- Males can have sperm banking done at The University of Kansas Cancer Center. For additional information or to set up an appointment, please call (913) 588-2229. (913-588-BABY)
- Premature menopause:
- Can occur after conditioning chemotherapy and/or radiation.
- For women you may not have menstrual periods or be able to become pregnant naturally after transplant.
- If you are interested in embryo freezing please talk with your physician right away. For additional information or to set up an appointment, please call (913) 588-2229. (913-588-BABY)
- Fatigue
- Can occur with chemotherapy or radiation
- Can last for a long time after transplant
Receiving Your Stem Cell Transplant
You will be given your stem cells after getting your pre-transplant conditioning chemotherapy. There will be several medical staff members involved. A laboratory scientist will thaw your cells and a nurse will infuse them. The nurse will take frequent vital signs. The infusion will take 2-5 hours. During the reinfusion of your stem cells you may feel nausea, chest heaviness, flushing or an unusual taste. These sensations don’t last long and can be treated quickly.
Your transplant is described by the care team using a timeline. The day you receive your stem cells is called “day 0.” The days before you receive your stem cells are “minus” days and the days after you receive your stem cells are “plus” days. For example, patients may start their pre-transplant conditioning chemotherapy on Day -6, which is 6 days before receiving your cells. Four days after you receive your transplant will be Day +4.
Waiting for Engraftment
Engraftment is when your body accepts the transplant and your white blood cell counts start to return to normal. White blood cell engraftment usually occurs 2-3 weeks after your transplant. This may vary depending on your disease and treatment. Usually the first sign of engraftment is a rising white blood cell count. Platelets and red blood cells usually take longer than white blood cells to recover. The actual time for recovery of all cells will vary from person to person.
While watching for the first signs of engraftment, you will require careful monitoring by nursing and medical staff. They will support you until you are producing blood cells again, to provide quick treatment if complications occur, and to prevent and treat infections.
After Engraftment
After engraftment, your immune system will continue to grow. Your care team’s goal is to support your recovery and treat any complications that happen during this phase. You must remain in the Kansas City area for about 100 days after transplant. You will have many restrictions to help prevent you from getting an infection. The BMT physicians will continue to see you, but may also involve the provider who referred you.